I’m a 64 year-old road/trail runner, marathoner and weight lifter diagnosed with atrial fibrillation more than a decade ago. I’ve had three ablations and as many cardioversions, plus I’ve swallowed the usual assortment of prescription meds. Now my a-fib has become paroxysmal atrial flutter—about one episode every two weeks or so, usually lasting a few hours—and while my running days seem to be over, I still regularly make it to the gym and I’m discovering the joys of walking and hiking.
Through trial and error—plenty of each, actually—as well as a fair amount of research, I’ve come to a handful of conclusions that may be useful. While I believe them to be true, keep in mind that my observations are true for me; your experience may well be different. Finally, since I’m not a physician, nothing here is intended as medical advice.
And now: 5 things I’ve learned in 10 years of dealing with the always-entertaining world of cardiac arrhythmia.
A-Fib won’t kill you…even though a diagnosis of a-fib—and its symptoms—can be very scary, barring underlying cardiac disease, a-fib is not inherently life-threatening. And so if you have just been diagnosed, relax as best you can.
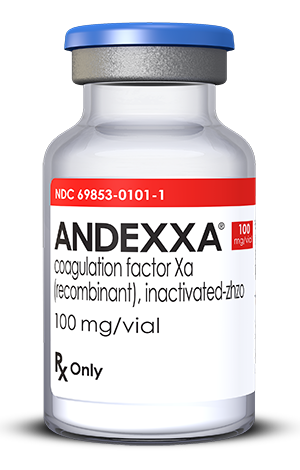
…but a stroke could. Pay rigorous attention to your anti-coagulation regimen. Even if your CHAD score is zero, at least take a low-dose aspirin every day. Personally, I find Coumadin to be a true pain, what with blood monitoring, dietary restrictions and the like. I much prefer the newer meds, especially Xarelto. It acts quickly, and as an added bonus you don’t have to be continuously concerned with your INR numbers.

Your EP isn’t interested in prevention. Typically, EP’s are all about fixing stuff rather than prevention. Which is weird, because unless you’re on the younger side of 40 and/or your a-fib has been freshly discovered, one ablation usually won’t do the trick. Of course, I’m grateful to my two EP’s, one rated among the best in California and the other acknowledged as one of the best in the world. It’s just that neither one has ever expressed any interest in the contours of my life, including what my exercise habits happen to be, what sorts of supplements I take, or what my days are like. Now, I’m not looking for a new best friend, but it’s clear that for them I’m a unique problem to be solved rather than a unique human being. I’m not angry about it; after all, these docs chose a field in which their major interaction with patients occurs when the patient is unconscious.
Still, I believe the implication is clear: you are pretty much on your own when it comes to figuring out how to modify your life style, exploring vitamin/mineral supplementation, and gathering the latest non-nutsy information.
(BTW, in terms of info, two websites I recommend are Dr. John Madrola and The A-Fib Report. Dr. John is a younger EP who always has a thought provoking take on new developments in a-f treatment and research and The A-Fib Report is a readable compendium of international a-f research, written in lay language. It requires a nominal membership fee that’s well worth it.)

Supplementation could work for you. I haven’t thrown out my beta blocker (Sotalol AF, not regular Sotalol) but along the way I have had excellent results in controlling the frequency and duration of my atrial flutter episodes by supplementing with 200 mg of magnesium citrate in a pill taken at lunch and ¼ teaspoon of potassium citrate dissolved in water taken in the morning and again at dinnertime (Please note: ingesting too much potassium involves some quite severe health risks, so be careful.)
Life is good. But first, the bad news: as near as I can tell, nobody knows what causes atrial flutter. The gang of suspects spans endurance sports (!) to mysterious biochemical mechanisms that somehow encourage the formation of tissue substrates that make the electrical system of the heart go haywire. Researchers—and your EP, too–are just guessing, leaning on statistical correlations rather than employing demonstrable causal connections. Maybe cutting out caffeine will help you; maybe it won’t. Maybe abstaining from demon rum will prove to be the answer; maybe not. Obviously, if you are over-drinking, over stressing (like many of us who are into enduro sports) under sleeping or happen to be engaged in other deleterious deeds, changing your behavior is simply a good idea, a-fib or no a-fib. Just don’t expect that any one thing will be the answer.
The good news is, you can have a great life even with a-fib and a-flutter. No, I don’t love my a-flutter episodes; they are annoying and sometimes, even after a decade, still frightening. I don’t run anymore, but a long walk or a moderate—I know, I know, not my favorite word, either—hike turns out to be a lot of fun. No, I can’t put the same hemodynamic load on my heart that I used to, but I can still work up a nice funky sweat underneath the weight machines at the gym.

Besides, working out is only a part of life. My friendships, relationship with my son, work, and my love life (I’m getting married again, and I’m stoked!) are just as satisfying as ever.
Maybe more so.
Those of us with a-fib or a-flutter aren’t sick, not truly. Nor do we need to afraid.
So—live!
(Thanks to Linda for the inspiration. Thanks to you for reading.)